Orthopedic surgeries can require a follow-up with regenerative intra-articular medications to help assist healing and to decrease the risk of further degeneration from biologic mediators. In arthroscopy procedures a bone fragment or weak detached or attached cartilage is removed from a particular joint space as a treatment for lameness, joint effusion, or suspect future unsoundness. Post-surgical aftercare requires an extended rest period that slowly develops into a gradual rehabilitation period towards normal workload. During the post-surgical period of rest, regenerative therapies are recommended for joints otherwise compromised by degenerative changes brought on by the primary disease process, namely bone fragments, and by intervention of surgical instruments. Currently, there are two widely used choices for regenerative intra-articular medications. IRAP and PRP are beneficial adjuncts during the post-surgical period following an arthroscopy.
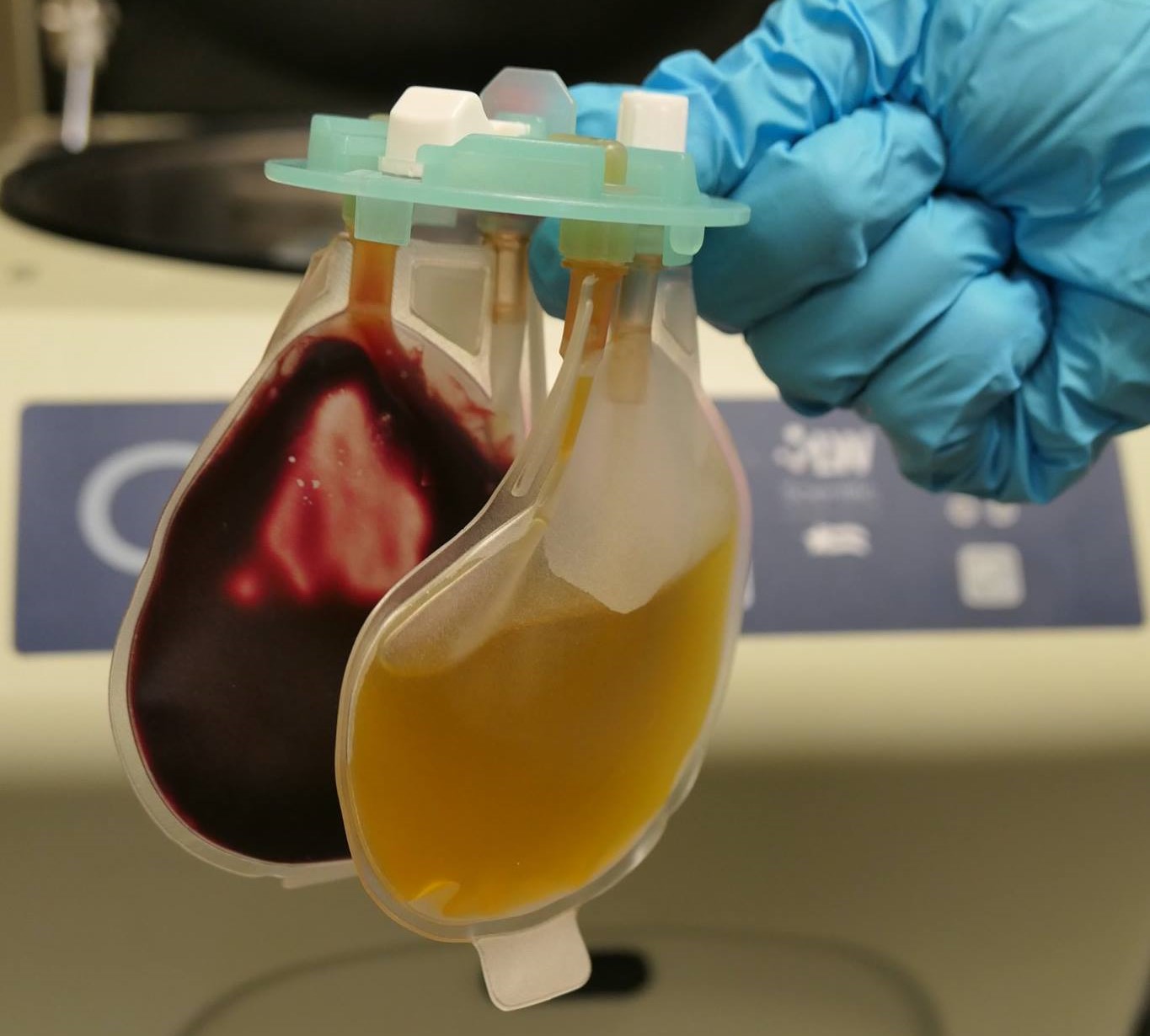
IRAP, or Interleukin-1 Antagonist Protein, are proteins derived from our horse’s own blood, that is processed and injected back into the affected joint to inhibit or prevent the progression of arthritis by actually blocking the receptors that the inflammatory mediator, Interleulin -1, would otherwise attach to in order to promote an inflammatory response. IRAP therapy is designed as a three-injection protocol – one injection monthly, with subsequent samples frozen until use.
PRP, or Platelet-Rich Plasma, has traditionally been used as a regenerative therapy to repair soft tissue lesions, but as processing techniques have advanced, intra-articular use has proven to be beneficial. In the joint, PRP promotes growth factors that help heal synovial (joint) fluid, and in turn provides an analgesic or pain relief effect to the joint. While single PRP injections in soft tissue lesions are recommended, a three-injection series is recommended for post-surgical cases or a joint compromised by severe arthritis. Process time for PRP is only 10 minutes versus IRAP that takes 24 hours.